For Dental and Vision Networks
PROVIDING SMARTER MANAGEMENT FOR TODAY’S DENTAL AND VISION PLANS

THE LEADING PROVIDER NETWORK MANAGEMENT PARTNER
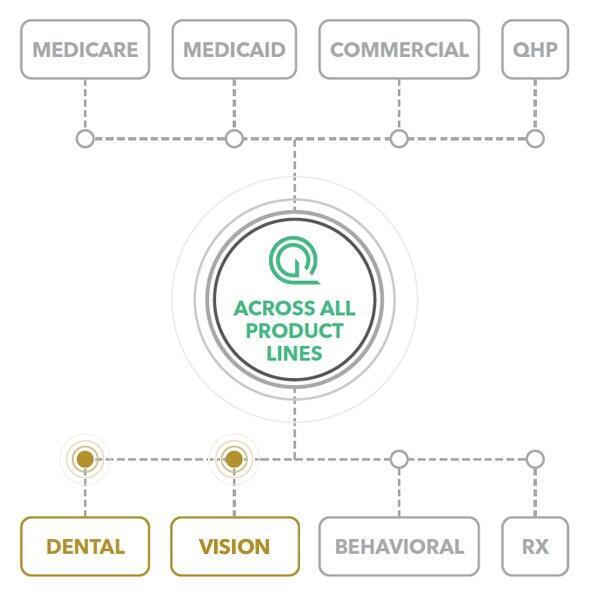
Quest Analytics helps America’s leading dental and vision plans measure, manage and monitor network performance across all business lines.
Our Quest Enterprise Services links network adequacy and provider directory accuracy thereby reducing regulatory risk for both measures, while allowing you to integrate actionable data and insights within your workflow, including credentialing, directories, contracting, claims and more.
NETWORK ADEQUACY AND PROVIDER ACCURACY FOR YOUR DENTAL AND VISION NETWORKS

RESPOND CONFIDENTLY TO RFPS

RESPOND CONFIDENTLY TO ACCREDITATION REQUESTS
QUEST DENTAL AND VISION SERVICES
Provide access to the tools and insights your team needs to work more intelligently and more proactively.
TO HELP YOU ENSURE YOUR MEMBERS HAVE ADEQUATE ACCESS TO CARE, OUR SERVICES INCLUDE:
1. Competitive Advantage RFPs
2. Provider Data Management Services
3. Market Comparisons
4. Membership Analysis
5. Network Performance Trending
6. Adequacy Services
7. Accuracy Services
8. Impact Analysis Services
ADEQUACY + ACCURACY IN ONE PLATFORM
SOLVE YOUR PROVIDER DIRECTORY ACCURACY CHALLENGES TODAY
Our team is ready to help you address the challenges provider data presents. We want to help you take your member experiences to the next level and avoid regulatory risks, like audits, and meet the mandates around surprise billing.
Contact us today to book a strategy session to understand and provide guidance to limit your exposure.