Don’t be surprised – be prepared for the new provider directory verification mandate listed in the No Surprises Act.
The No Surprises Act ended surprise medical bills for patients and enacted new provider directory verification mandates, including requirements for both health plans and providers. Our industry-expert speakers answer the top questions pertinent to the regulatory requirements focused on how health plans and providers should prepare for the requirements scheduled to take effect on January 1, 2022. You will also learn best practices, strategies, and actionable steps you can take today to align with the new federal requirements.
You don’t want to miss this (and we don’t want you to miss it either)!
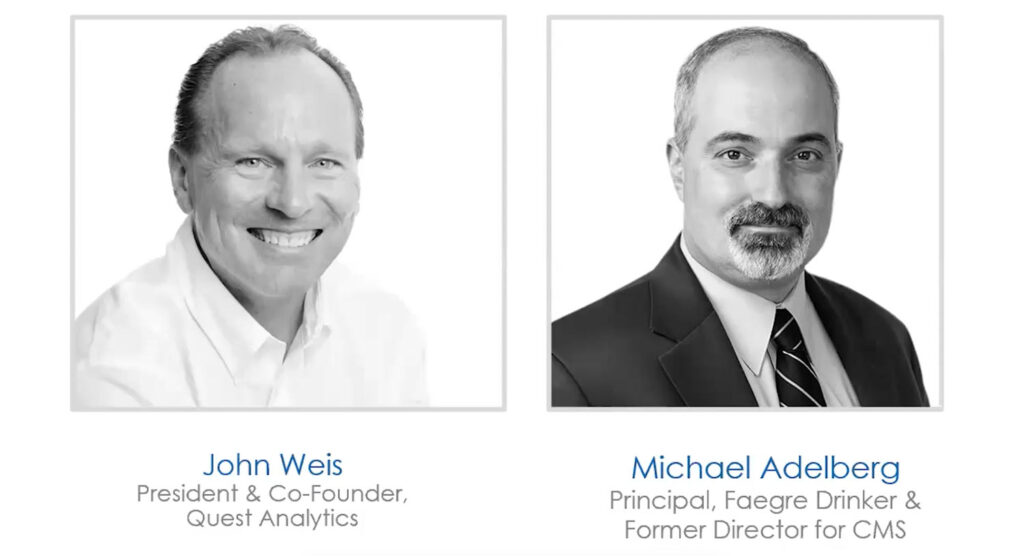
Panelists:
John Weis, President and Co-Founder, Quest Analytics
Michael Adelberg, Principal, Faegre Drinker Consulting and Former Director for CMS
Moderator: April Beane, Senior Director of Marketing, Quest Analytics
View The Recording
MORE SURPRISE BILLING PROVIDER DIRECTORY ACCURACY RESOURCES
Quest Analytics is your one-stop shop to help you prepare for the new Provider Directory Information and Provider Requirements, listed in the No Surprises Act – Protecting Patients and Improving the Accuracy of the Provider Directory Information. Explore our No Surprises Act Resource Center to stay up-to-date on the provider directory verification requirements, find preparation guides and videos to help you develop a strategic plan to meet deadlines, and learn about the solutions that can get you there quickly.
Deliver on tomorrow's goals by planning today
We are committed to assisting our customers in their quest for accurate provider directories and adequate health networks that maintain appropriate access to care for your members.