More insider information on how to comply with No Surprises Act provider data accuracy requirements.
A process isn’t a process unless it’s documented. That’s especially true when it comes to health plan compliance. We’ve seen this play out with Medicare Advantage Network Adequacy Audits and now we’re seeing it with the No Surprises Act Provider Directory Requirements. The No Surprises Act requires health plans to have a documented, defendable process to show their efforts in establishing and maintaining an accurate provider directory. Although regulators are still polishing up elements of the rule, one thing is certain: they will be looking for proof that you’re taking all the necessary steps to comply.
To give you an edge, we’re spilling the beans on how to create a provider data management workflow that will pass muster with the powers that be.
Creating Your Provider Data Management Process
Set Up A Three-Tier System For Categorizing Your Providers
It’s easy to feel like there are a million and one different ways you could go about designing a provider data management process. You might be feeling overwhelmed and asking yourself, “What if my approach isn’t accepted by a regulator?” Don’t worry because we’ve got your back!
Our amazing Regulatory Team has done all the legwork for you and created a workflow that will make sure you’re compliant with all the No Surprises Act requirements. And the best part? It’s easy to incorporate into your existing processes, so you don’t have to reinvent the wheel.
To begin, create a three-tier system to categorize the providers in your database.
- Providers who remain in the directory.
- Providers who remain in the directory but you’ll want to flag.
- Providers who do not stay in the directory.
Now, let’s dive into the data workflow even further to make sure you have a strong, reliable process in place. All you have to do is follow the steps and you’ll be good to go!
Tier One: Providers Who Remain In the Directory
The No Surprises Act stipulates that health plans must have a process in place to verify and update the provider directory information at least every 90 days1 for each provider and healthcare facility included in the database. Providers and facilities who verify their information as required and the information they provide does not raise concerns, stay in the provider directory.
Tier Two: Providers Who Remain In the Directory, But Should be Flagged
What happens when you have providers or facilities who verify the information within the required timeframe, but some of the responses are questionable? You can add them to the directory. However, don’t stop there. We strongly suggest you flag and research the suspect responses to ensure the data you provide is reliable and accurate. Doing this will give you the peace of mind that the information you present in your directory and database is trustworthy.

Tier Three: Providers Who Do Not Stay in the directory
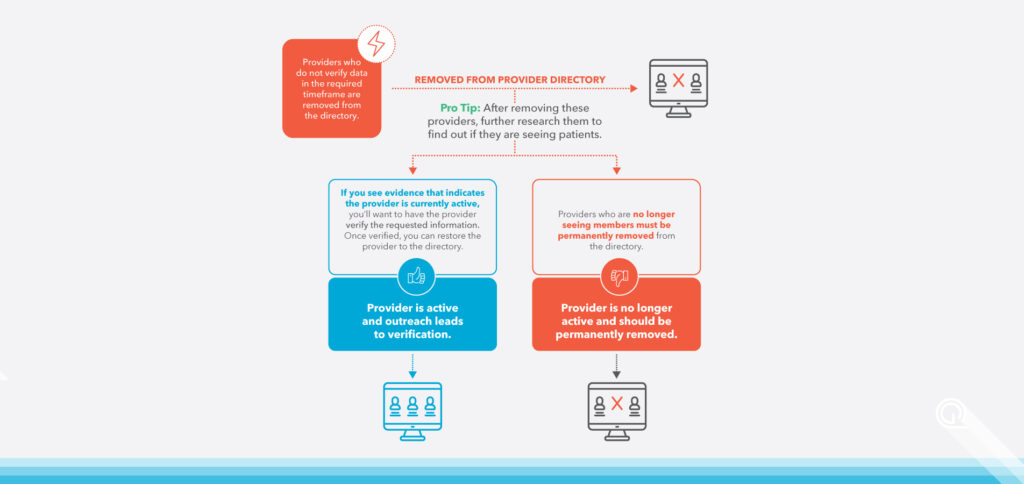
Now that you know when to keep providers in th directory, let’s walk through what you should do when you need to remove providers from the directory. When providers fail to verify their data in the required timeframe, they must be removed from the directory. This removal is done in order to ensure that the directory remains up-to-date with the correct information regarding your network.
Don’t settle for just that. After removing these providers, further research should be done to find out if they are actively seeing patients.
For example, if you see evidence that indicates the provider is active, you’ll want to take additional steps to have the provider verify the requested information. Once verified, you can restore the provider to the directory.
If you determine the provider is no longer practicing, the provider must be permanently removed from the directory.
Quest Analytics Makes Data Management Easier
Let Quest Analytics Help You Create a Provider Data Management Process That’s Right for Your Business
With Quest Enterprise Services, you gain the tools you need to establish a provider data verification process that’s right for your business. Whether you’re looking for a quick snapshot of the latest changes in your data, needing to take a deep dive into provider information, or wanting an easier way to make strategic decisions about your network, we have you covered.
- Compliance Monitoring
- Provider Data Management
- Network Modeling
- Provider Impact Analysis
- Automated Actionable Analytics
- Project Oversight & Guidance
- Accuracy API
- Volume Actions
And our clients benefit from our team partnership. We do the heavy lifting of data management, outreach and analysis so that you can spend your time focusing on what really matters: making sure your provider directory is ready for prime time!

Save Time, Stay Compliant
Experience the convenience of streamlining provider data accuracy with Quest Enterprise Services! Our powerful API ensures that your provider data is compliant and up to date, so you can focus on the bigger picture. With Quest Enterprise Services, you can save time and stay compliant – just one more reason to get all your teams on board.
Upgrade your provider data and network management processes today with Quest Enterprise Services!
More Provider Data Management Tips
Footnotes
- The No Surprises Act requires health plans to verify all provider directory data every 90 days, process updates within two business days of receiving updated information and remove providers from the directory if their information has not been verified during a period specified by the health plan. Print directories must include the date of the last update. At the same time, providers and facilities must have a process in place to provide the health plan with timely provisions of directory information.