FAQs and Provider Directory Requirements: Key Tips and Targets

One of the top questions health insurers have asked us lately is: Will I still need to have a provider directory verification process in place by January 1, 2022? Simply put, yes. In this blog, we’re highlighting the essential points you need to know about the FAQs and provider directory requirements. FAQS ABOUT THE PROVIDER DIRECTORY REQUIREMENTS […]
New Guidance on Provider Directory Verification Requirements Stands Firm on January 1, 2022, Effective Date

In a new guidance document that provided plans and issuers with some enforcement delays over key new price transparency requirements, the Biden administration stood firm on new provider directory verification requirements effective January 1, 2022. BACKGROUND As discussed in a prior post from Quest Analytics, starting on January 1, 2022, section 116 of the Consolidated Appropriations […]
Federal Update: Requirements Related to Surprise Billing; Part 1

On July 1, the Biden administration released an interim final rule with comment period (IFC), “Requirements Related to Surprise Billing; Part I.” This is the first significant step to implementing the No Surprises Act, passed as part of the Consolidated Appropriations Act of 2021 (CAA) in December 2020. The No Surprises Act protects healthcare consumers, […]
Surprises in the No Surprises Act: New Requirements for Plans and Providers Regarding Provider Directory Information

Copyright 2021 Compliance Today, a publication of the Health Care Compliance Association (HCCA). The No Surprises Act was signed into law in December 2020 as part of the massive Consolidated Appropriations Act of 2021.[1] It is the end result of several prior bills that sought to address the national “surprise bill” problem. In recent years, millions […]
Top 3 Things the “No Surprises Act” Means for Health Plans
It’s staggering to think that, according to researchers, one in five emergency room visits result in an individual receiving a bill for treatment or services they expected to be covered by their health plan, but weren’t. These unexpected, costly, and often frustrating charges are aptly called Surprise Medical Bills. While surprise medical bills impact consumers financially, […]
Designing and Building Clinician Networks That Address Social Determinants of Health
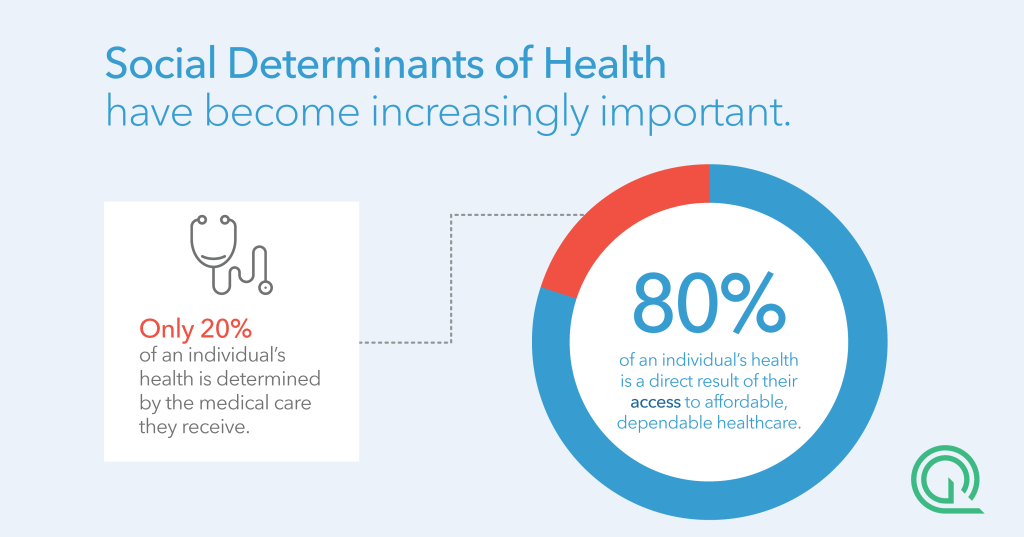
FIVE TAKEAWAYS FROM OUR WEBINAR Watch: Designing and Building Clinician Networks That Address Social Determinants of Health As clinicians and payers take on increasing risk for patient outcomes, it is essential that leaders consider the effectiveness of their networks as well as the accuracy of their clinician directories to ensure they are adequately serving their members. Modern […]
5 Things I Learned at Vision Quest

Admittedly, I’m new to provider network management. I’ve spent years working in healthcare, but this is my first time working with payers from across the nation to improve the access, adequacy, and accuracy of their provider networks. Lucky for me, I got a behind-the-scenes view through Quest Analytics Vision Quest. As a session moderator, I heard […]
Preparing for the Era of Provider Network Transparency

Copyright 2020 Compliance Today, a publication of the Health Care Compliance Association (HCCA). Transparency is one of the top buzzwords in healthcare today. In the last few years, we have seen the rollout of significant healthcare transparency initiatives focused on portable health records, hospital costs, drug costs, quality data, and many other things (e.g., Executive […]
Rule Raises Questions About Telehealth, Directory Accuracy

Reprinted with AIS Health permission from the July 2, 2020, issue of RADAR on Medicare Advantage. As Medicare Advantage and other insurers report increasing use of telehealth during the COVID-19 pandemic and consider the larger role that virtual visits could play on a more permanent basis, CMS recently finalized a set of policies for 2021 […]
Quest Analytics Launches Quest Enterprise Services
First to launch platform enabling health plans to simultaneously measure, manage and monitor network adequacy AND directory accuracy. OVERLAND PARK, Kan., June 16, 2020 – Quest Analytics, the leader in measuring, managing and monitoring health plan network performance, today announced the release of Quest Enterprise Services (QES), the first and only platform to enable the health plan community to […]