Medicare Advantage
Compliance may not be our name, but it’s definitely our game. Our relationship with CMS—the people who set the standards we all follow—means we can help you be compliant. Visit our CMS Resource Hub to find guides, videos, and more!
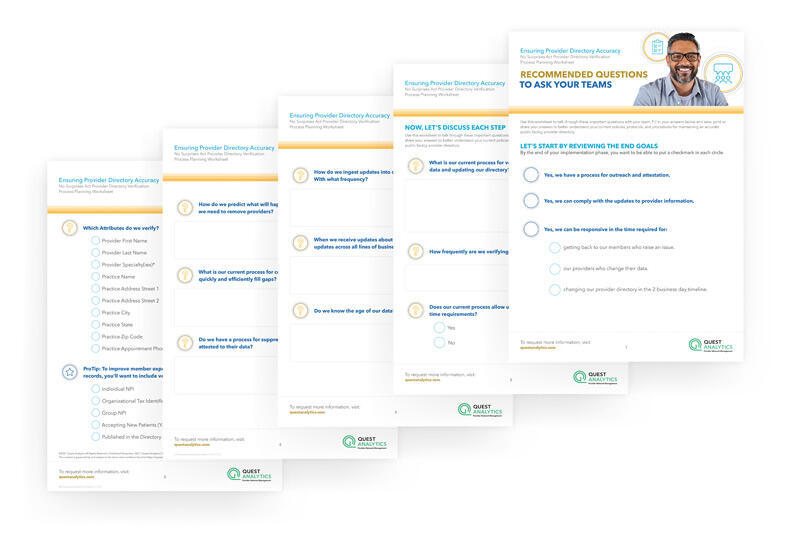
Provider Directory Accuracy
Stay ahead of the game with help from our Surprise Billing Resource Hub. You’ll find the latest insights, videos, guides and more to help you be compliant with the provider directory verification requirements.

QHP Certification
New network adequacy requirements for Qualified Health Plans (QHPs) on the Federal Exchange. Go to our QHP Marketplace Resource Hub to get all the details on what’s new and how you can prepare today!
FIND THE SOLUTION THAT’S RIGHT FOR YOU

QES Adequacy & Accuracy
Get industry-leading compliance capabilities that enable you to meet numerous federal and state healthcare mandates, including the No Surprises Act and Medicare Advantage.

Medicare Advantage
CMS Network Adequacy Compliance year-round. With QES Adequacy, you measure your network as CMS will – giving you a superior way to maintain compliance for current and future networks.

Federal & State Templates
Say goodbye to manual project set-up and say hello to peace of mind. Our pre-built Federal and State templates allow you to skip the manual work and measure your network as regulators will.

QES Access Reporting
Generate multiple access reports in minutes! Plus, quickly report on any size business, giving your Sales Team a competitive advantage in the Small Group Market.

Commercial Networks
Helping you create competitive advantages in the marketplace. Plus, measure your network for URAC and NCQA network adequacy accreditation.
Dental Networks
Quest Enterprise Services provides complete and automated visibility into your network, allowing you to make informed decisions quickly.
- 00Days
- 00Hours
- 00Minutes
- 00Seconds