- WHO We Help
- Payers & PlansHealth SystemsSpecialtiesRegulators
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Medicare Advantage
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Medicaid
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Commercial
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
QHP
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Acute & Post-Acute Care
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
PCP
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Specialty
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Ancillary Care
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Dental
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Vision
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
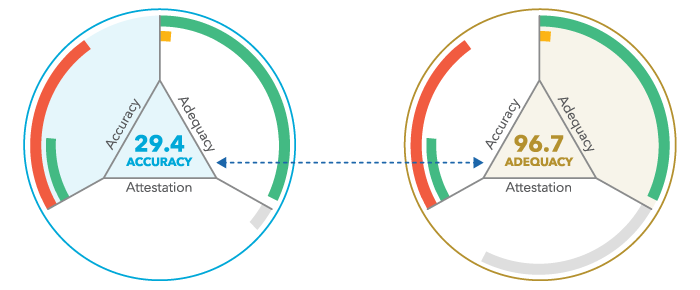
Network Accuracy
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
State
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Federal
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Regulatory Review
- HOW We Help
- Quest Enterprise Services (QES)Quest Analytics Suite (QAS)BetterDoctor
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Data Integrity
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Compliance
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Performance
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Efficiency
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Quest Analytics Suite (QAS)
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
QES Access Reporting
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
GeoAccess
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
L

BetterDoctor: Verfied Provider Directory Data
HELPING BUILD BETTER MEMBER EXPERIENCES
BetterDoctor is the only primary-sourced verified provider directory data solution that brings together verified data sources, like the National Plan and Provider Enumeration System (NPPES), the Office of Inspector General (OIG) and other proprietary sources, outreach to provider locations and attested provider data for individual practitioners as well as large groups that connects directly into Quest Enterprise Services Accuracy solution.
- Resources
- What’s HotResources ForTopicsDocuments
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Static Content Here
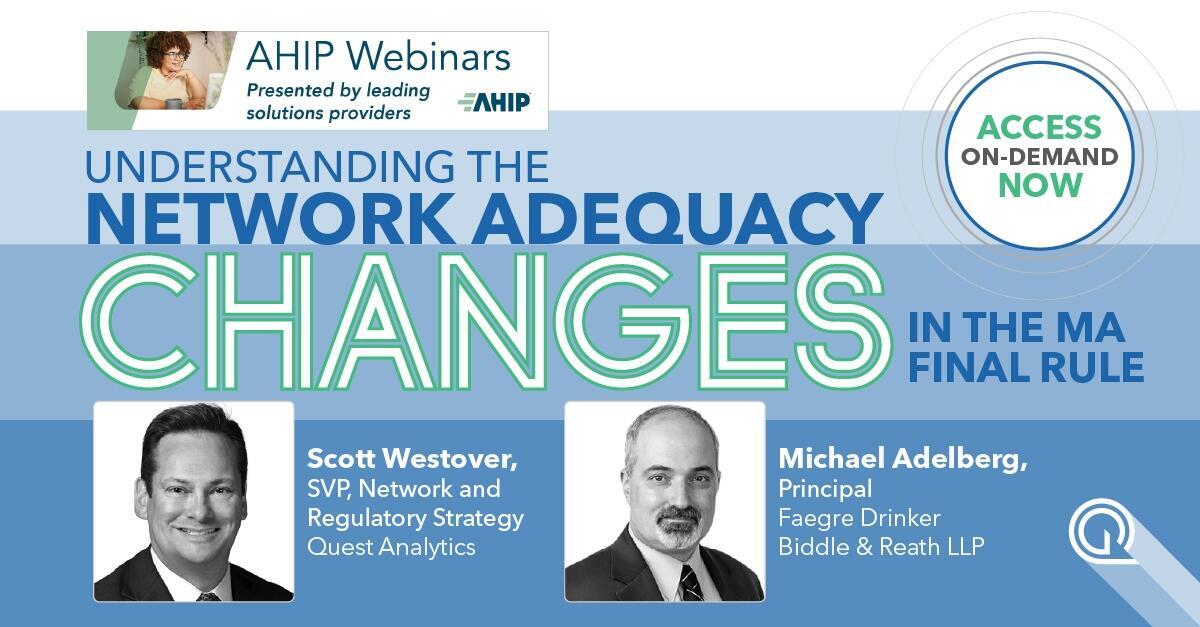
Here’s How You Can Prepare for the No Surprises ActMore insider information on how to comply with No Surprises Act provider data accuracy requirements. A process isn’t a process unless it’s documented. That’s especially true when it comes to...Here’s How You Can Prepare for the No Surprises ActMore insider information on how to comply with No Surprises Act provider data accuracy requirements. A process isn’t a process unless it’s documented. That’s especially true when it comes to...New Features to Improve Compliance with Federal RegulationsOVERLAND PARK, KS (June 30, 2022) – Quest Analytics, the leader in provider network management solutions and services, today introduced three new features for Quest Enterprise Services (QES) designed to improve their client’s ability...Quest Analytics Launches QES Access ReportingOVERLAND PARK, KS (June 22, 2022) – Quest Analytics, the leader in provider network management solutions and services, today launched the company’s newest software innovation, Quest Enterprise Services (QES) Access Reporting, at AHIP 2022 in...Quest Analytics to Attend and Speak at AHIP 2022OVERLAND PARK, KS (June 21, 2022) – Quest Analytics, the leader in provider network management solutions and services, today announced that the company will attend AHIP 2022. At the conference, Quest Analytics will...Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Payers and Plans
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Regulators
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Health Systems
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Ancillary
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Lorem ipsum dolor sit
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Building Their Own HMOWanting to set up their own HMO, they needed to build a county-wide Medicare Advantage network — with no previous experience managing CMS network adequacy requirementsOversight, Meet InsightThey had manual oversight of provider network adequacy—but zero insight into provider availability, provider data accuracy or performance across health plans.“Are We Compliant — or Not?”They had no effective way to find their own adequacy gaps — but CMS and state regulators were finding plentyGrowing Nowhere FastTo quickly expand multiple lines of business into new counties and states, the health plan needed a faster, easier, and more cost-effective way to build adequate networks.More Than Meets the ROIA costly CMS penalty proved they couldn’t keep managing their provider networks the same old way. For a New York health plan, smarter provider network management was a better investment...A Tale of Two NetworksHaving struggled to build a Medicaid network, they now faced the more complex requirements of Medicare — with only one shot to get it right.Too Bad to Ignore, Too Big to FixProvider data accuracy issues could have jeopardized their partner relationships — but they didn’t have an effective way to address them.The Best Offense WinsTheir team was looking for automated and integrated tools and insights that would allow them to better communicate the value of their Integrated Delivery Network, by specialty, with an end...ROI
- About Us
- About UsCareersNewsEvents
l

Quest Analytics is the solution trusted by Payers, Providers and Regulators for Achieving Compelling and compliant healthcare networks.
Book A Strategy Session
Passionate, and Mission-Ready.

WHAT’S GOING ON AT QUEST ANALYTICS
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Here’s How You Can Prepare for the No Surprises ActMore insider information on how to comply with No Surprises Act provider data accuracy requirements. A process isn’t a process unless it’s documented. That’s especially true when it comes to...New Features to Improve Compliance with Federal RegulationsOVERLAND PARK, KS (June 30, 2022) – Quest Analytics, the leader in provider network management solutions and services, today introduced three new features for Quest Enterprise Services (QES) designed to improve their client’s ability...Quest Analytics Launches QES Access ReportingOVERLAND PARK, KS (June 22, 2022) – Quest Analytics, the leader in provider network management solutions and services, today launched the company’s newest software innovation, Quest Enterprise Services (QES) Access Reporting, at AHIP 2022 in...Quest Analytics to Attend and Speak at AHIP 2022OVERLAND PARK, KS (June 21, 2022) – Quest Analytics, the leader in provider network management solutions and services, today announced that the company will attend AHIP 2022. At the conference, Quest Analytics will...THIS IS WHERE WE WILL BE
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis vitae nibh sed hendrerit. Nulla vitae massa placerat nisi euismod convallis sit amet non quam.
Here’s How You Can Prepare for the No Surprises ActMore insider information on how to comply with No Surprises Act provider data accuracy requirements. A process isn’t a process unless it’s documented. That’s especially true when it comes to...New Features to Improve Compliance with Federal RegulationsOVERLAND PARK, KS (June 30, 2022) – Quest Analytics, the leader in provider network management solutions and services, today introduced three new features for Quest Enterprise Services (QES) designed to improve their client’s ability...Quest Analytics Launches QES Access ReportingOVERLAND PARK, KS (June 22, 2022) – Quest Analytics, the leader in provider network management solutions and services, today launched the company’s newest software innovation, Quest Enterprise Services (QES) Access Reporting, at AHIP 2022 in...Quest Analytics to Attend and Speak at AHIP 2022OVERLAND PARK, KS (June 21, 2022) – Quest Analytics, the leader in provider network management solutions and services, today announced that the company will attend AHIP 2022. At the conference, Quest Analytics will...
- Who We Help
- ACCESS TO CARE STARTS HERE
We help 90% of all healthcare networks deliver quality access to care — from Payers to Health Systems to Providers and Regulators — find out how we can help you!
- How We Help
- For ProvidersNetwork Performance Service
Gain a holistic view of the market and your network providers’ viability to your members, including their impact on your network adequacy – something only Quest Analytics can provide.
- About Us
- We Are HiringAbout UsEvents We Are A Part OfBE A QUESTER
We’re hiring. If you’re looking to use your talents to make a difference in the lives of healthcare consumers – we want to hear from you.
- Resources
- Featured ResourcesCase StudiesUNITING AN ENTERPRISE
Informed decisions on provider participation to ensure network optimization, speed to market, regulatory compliance and member satisfaction